Imagine waking up to a day only to find weakness in your limbs, such as your legs may not be ready to move according to the regular pattern. Some days pass on, and weaknesses become so worse that even simpler things are considered impossible to accomplish.
It is Guillain-Barré Syndrome (GBS), a serious but rare illness in which your body’s defenses mistakenly attack it. GBS can arise anytime and become critically worse in some time. Symptoms include tingling, muscle weaknesses, and, in severe cases, paralysis.
In its most severe form, it can severely paralyze the breathing ability and cause major problems that require emergency treatment in hospitals. The cause of GBS is unknown, but often follows infections such as flu or food poisoning. Now, the good news is that with suitable treatment, most patients recover, though it can take weeks, months, or even longer. In GBS cases, medical care and therapy help patients regains their strength and movements over time.
In this guide, we will talk about GB syndrome and its treatment. To dive into the depth of the topic, keep reading.
What is Guillain-Barre Syndrome?
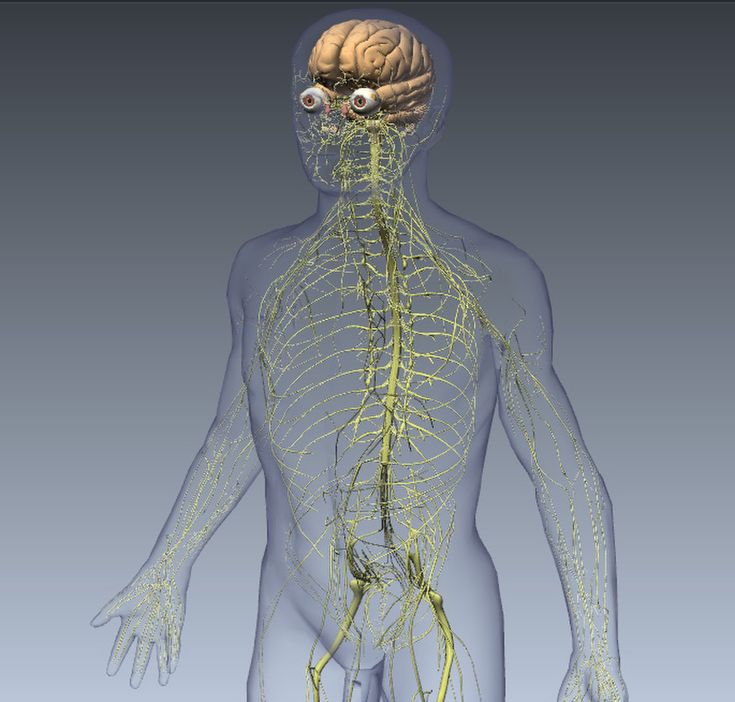
Guillian-Barre syndrome is a rare but major nerve condition that can attack anyone; the condition occurs when the body immune system-the immune system that in normal circumstances always protects the body against germs-mistakenly attacks the nerves outside of the brain and spinal cord.
Damage caused by this attacks the signals transmitted between the brain and the rest of the body, causing a weakening of such signals to manifest muscle weakness, tingling, numbness, and in worst cases, paralysis. Physicians aren’t quite certain what triggers GBS, though it is quite often that cases occur after having an infection.
Common infections reported to be connected with the beginning of GBS include respiratory, flu, and stomach infection. The signs may begin as mere weakness in legs and extend up to the remaining parts of the body. It is, though, pretty dreadful, and patients can easily make a complete recovery with appropriate treatment. Treatment and therapy help patients regain their strength, though recovery may take weeks, months, or even longer.
Types of Guillain-Barre Syndrome
Based on its unique characteristics, Guillain-Barre syndrome (GBS) can be divided into several subgroups. There are two primary kinds:
AIDP (Acute Inflammatory Demyelinating Polyneuropathy)
About 85% of all instances of Guillain-Barre syndrome are of this type. The fatty covering of nerve fibers, known as the myelin sheath, is attacked in the AIDP variant of Guillain-Barre syndrome. The nerve can no longer transmit the signal if the myelin sheath is destroyed, which results in weakness and other neurologic symptoms.
MFS (Miller Fisher Syndrome)
These have the less frequent form of GBS, affecting 5 to 10%. Three symptoms in total define this as MFS: ataxia (or lack of coordination), ophthalmoplegia-paralysis of muscles around the eye, and areflexia-parentheses indicating a loss of reflexes. In contrast with AIDP, MFS typically does not lead to muscle weakness in extremities. Other less prevalent variations and overlapping forms of Guillain-Barre syndrome exist in addition to these main categories, including:
Acute Motor Axonal Neuropathy (AMAN):
It mainly presents as Guillain-Barré Syndrome, affecting especially the nerves in charge of movement. This will cause weakness of the muscles but does not disturb the sensation of touch and pain. AMAN is often associated with infections due to some bacteria such as Campylobacter jejuni.
Acute Motor Sensory Axonal Neuropathy (AMSAN):
AMSAN is similar to AMAN in the respect that it affects both movement and sensation. Affected persons have muscle weakness that accompanies numbness or tingling sensation. This disease also, like AMAN, is connected with infections.
Acute Panautonomic Neuropathy:
This is a very rare presentation of Guillain-Barré Syndrome, where there is autonomic nervous system impairment related to activities like heart rate, blood pressure, and digestion. This easily presents as if people couldn’t even get simple things going in their body, such as being stable in heart rhythm or with digestion.
Causes and Risk Factors of Guillain-Barré Syndrome (GBS)
The exact source of Guillain-Barré syndrome is unknown, but typically it follows some kind of infection. The key causes and risk factors include:
Infections
GBS often follows an infection, most commonly a gastrointestinal or respiratory infection. The immune system may inadvertently target peripheral nerves as a response to the illness. Some of the illnesses associated with GBS include:
Campylobacter Jejuni: A common bacterium that causes food poisoning.
Cytomegalovirus (CMV): A member of the herpesvirus family.
Epstein-Barr Virus (EBV): Another herpesvirus, the one responsible for infectious mononucleosis.
Mycoplasma Pneumonia: An organism that is a causative agent of respiratory infections.
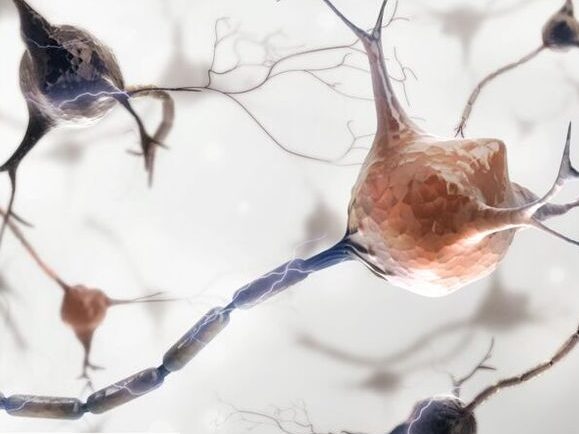
Immune Response
Guillain-Barré syndrome is an autoimmune disorder that develops due to an aberrant response by the immune system, in which it attacks the peripheral nerves by mistake. The mechanisms underlying such an immune response are intricate and not very well understood. A critical consideration in this regard is that even though certain infections and immunizations pose a higher risk for GBS, GBS is relatively a rare disease and most individuals exposed to such infections or receiving vaccines do not later develop GBS.
Vaccinations
There have been sporadic reports of GBS after some immunizations, including the swine flu and flu vaccines. The risk of getting GBS after vaccination, however, is generally considered to be extremely low compared with the risk of getting diseases naturally.
Other Factors
Other than infections and vaccines, some other things that might increase the chances of developing Guillain-Barré Syndrome (GBS) include:
Age and Gender: GBS can occur to anyone, although it is seen more in adults, especially elderly people. It is a little more common in men than in women.
Health Conditions: For example, several diseases have already been associated with GBS such as HIV/AIDS, lupus, and Hodgkin’s lymphoma.
Surgery or Injuries: At times, GBS has been associated with some surgery or very serious injuries although the doctors cannot establish the level of strength at which this might be connected.
Other Infections: Besides well-known infections, viruses like hepatitis A and Zika have also been linked to GBS in some people.
Guillain-Barré Syndrome Diagnosis
Diagnosis procedures for Guillain-Barré Syndrome (GBS) may include the use of any number of diagnostic tests, study of the patient’s medical history, and clinical examination. Since the outcome is highly dependent upon early detection and treatment, it is extremely important that anyone who is experiencing symptoms which suggest a case of GBS seek medical attention. The GBS diagnosis procedure might involve:
Clinical Evaluation
Medical History: The doctor will ask about the person’s past health, including any recent sickness or infections.
Physical Check-Up: The doctor will carefully check the person’s nerves and muscles to see how strong they are. They will also test reflexes, movement, and feeling in different parts of the body.
Electrodiagnostic Tests
Electromyography (EMG): EMG detects muscular electrical activity. Muscle activity abnormalities could be a sign of nerve injury.
Nerve Conduction Studies (NCS): As electrical impulses go via nerves, NCS measures their strength and speed. Because of damage to the myelin sheath or nerves, nerve transmission is frequently hindered or inhibited in GBS.
Blood Tests
Blood tests can be used to detect specific infectious triggers linked to GBS, such as antibodies against particular bacteria or viruses, or to rule out other illnesses that could mimic GBS.
Imaging Studies
Imaging tests such as magnetic resonance imaging (MRI) may be carried out to rule out alternative explanations of neurological symptoms, while they are usually not required for diagnosis.
Guillain-Barré Syndrome Treatment
You’ll receive immediate hospital treatment if you’ve been diagnosed with Guillain-Barré syndrome. Typically, your hospital stay would be for a few weeks. For a few months, some people might have to stay.
Immunotherapy is the primary treatment that will prevent your immune system from attacking your nerves. Intravenous immunoglobulin (IVIG) or plasma exchange will be administered to you.
To assist control your symptoms and keep an eye on your health, you will also receive treatment.
What you may need:
Medication and compression stockings to lower the risk of deep vein thrombosis (DVT); If you are unable to walk;
if you have serious breathing issues, you should be in an intensive care unit (ICU);
And if you are on a ventilator, amitriptyline, gabapentin, or carbamazepine
Plasma Exchange (Plasmapheresis): The process involves removal of the disease-causing antibodies from your plasma and replaced by fluids or fresh plasma. This treatment might be used when IVIG fails and the case is serious.
Corticosteroids: It may be combined with other medications for the decrease of inflammation as well as immune response suppression of the body.
Conclusion
GBs is a severe, but rare condition caused by your body’s immune system attacking the nerves. This can result in muscle weakness, tingling, and even paralysis. Although its cause is not known precisely, it frequently occurs after infection with such conditions as the flu or food poisoning. The diagnosis of GBS varies from one person to another, and there are different types of the syndrome. Although there is no cure for GBS, some treatments such as intravenous immunoglobulin (IVIG), plasma exchange, and other drugs can help to alleviate symptoms and improve recovery.
Most people suffering from GBS can recover properly with appropriate care, though recovery may take weeks or months. If you find any signs of GBS, you should get medical help immediately to start early treatment. Proper support and therapy can help a person regain their strength and get better over time.
FAQs (Frequently Asked Questions)
What is Guillain-Barré Syndrome (GBS)?
Guillain-Barré syndrome is a very rare disease wherein the immune system mistakenly attacks the nerves, resulting in weakness, numbness, and sometimes paralysis. This syndrome commonly develops as a complication of influenza or food poisoning.
What are the symptoms of GBS?
The syndrome has general symptoms of numbness, weakness of the muscles, and paresthesias. It is dangerous since paralysis develops followed by a cessation in breathing.
What causes GBS?
The exact cause is not known, but GBS often occurs following an infection like respiratory diseases, stomach infections, or viruses like the flu. In very rare cases, it can occur as a consequence of vaccines or surgery.
Can GBS be cured?
Most people get well, but some may suffer from long-term effects, like weakness in certain muscles, numbness, or even fatigue. The earlier prognosis and treatment, the more probable complete recovery.
Can GBS lead to permanent damage?
While most people recover, some may experience long-term effects such as muscle weakness, numbness, or fatigue. Early diagnosis and treatment improve the chances of a full recovery.

